The overuse of antibiotics, in people and animals, has led to the emergence of antibiotic-resistant bacteria or ‘superbugs’ which can cause infections that are difficult to treat. If antibiotics fail, chest infections, urinary tract infections (UTIs), cuts, insect bites and even small scratches can develop into sepsis (blood poisoning), which can be fatal.
The World Health Organisation (WHO) say that antimicrobial resistance (AMR) is one of the main threats to modern medicine with growing numbers of infections – such as pneumonia, tuberculosis, gonorrhoea and salmonellosis – becoming harder to treat. Drug resistance is already here, the WHO warns: “AMR affects countries in all regions and at all income levels. Its drivers and consequences are exacerbated by poverty and inequality, and low- and middle-income countries are most affected.”
AMR is an urgent global public health threat, killing at least 1.27 million people worldwide, which is included in the almost five million deaths associated with AMR in 2019. One in five of those deaths occurred among children under five years old. The number of people dying from AMR infections could rise to 10 million a year by 2050 if no action is taken to curb the overuse of antibiotics.
Growth promoter
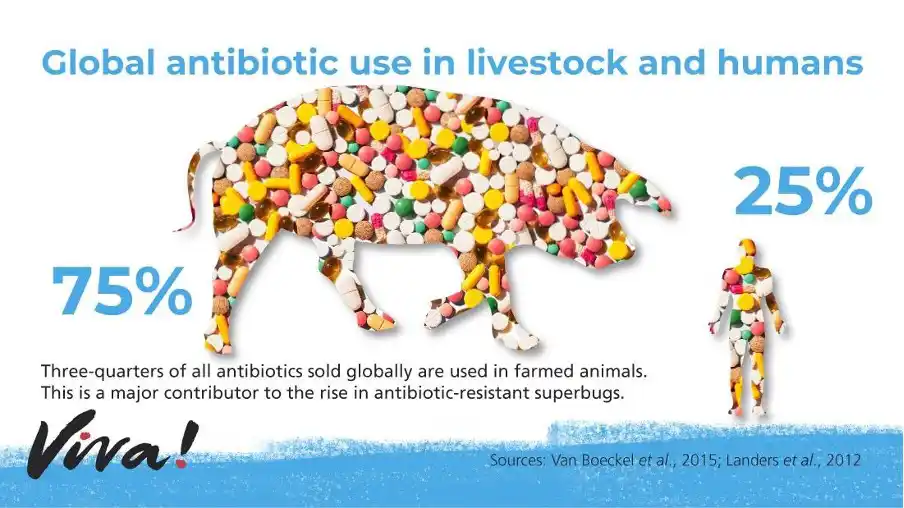
When used at low doses, antibiotics promote growth in farmed animals. This has led to their widespread use in farming around the world and it’s estimated that around 70 per cent of all antimicrobials sold globally are used in animals raised for food. It may be more, as many countries don’t report antimicrobial use in farmed animals and in many countries, their use continues to outweigh human use.
At least 41 countries still permit the use of medically important antibiotics as growth promoters in farmed animals according to the World Organisation of Animal Health (WOAH), who also say that many more countries, including the United States, still permit the use of non-medically important antibiotics as growth promoters. Furthermore, many countries continue to use antibiotics routinely in healthy animals to prevent disease. Both practices are driving the emergence of antibiotic-resistant bacteria.
AMR in Uganda
Antibiotic resistance is a growing problem in Uganda, just as it is in other countries. In Uganda in 2019, there were 7,100 deaths attributable to AMR and 30,700 deaths associated with it. The number of AMR deaths in Uganda is higher than deaths from respiratory infections and tuberculosis, cardiovascular diseases, HIV/AIDS and sexually transmitted infections, neglected tropical diseases (a diverse group of bacterial, viral and parasitic infectious diseases that disproportionately affect people living in poverty around the world), malaria and neoplasms, according to the Institute for Health Metrics and Evaluation (IHME).
As many as half of all bacterial infections in Uganda show resistance against commonly prescribed antibiotics such as penicillin, cephalosporins and tetracyclines. Multi-drug resistant bacteria, including methicillin-resistant Staphylococcus aureus (MRSA) are on the rise and these pathogens are showing increasing resistance to antibiotics that are generally reserved for difficult-to-treat multi-drug resistant infections.
The five main pathogens in Uganda (along with the number of deaths associated with AMR given in brackets) are Klebsiella pneumoniae (5,700), Streptococcus pneumoniae (5,100), Escherichia coli (4,200), Staphylococcus aureus (4,200) and Salmonella Typhi (1,800). These commonly cause lower respiratory infections and all related infections in the thorax (including heart and lungs), bloodstream infections and peritoneal and intraabdominal infections.
In 2018, Uganda developed a five-year AMR National Action Plan (NAP) which set out a framework of actions to address AMR in the country using a One Health approach. One of the aims was to improve knowledge and awareness of AMR among health practitioners, farmers and the general public. However, there is still limited information on antibiotic use both in animals and people. The estimated annual consumption of antimicrobials in Uganda in 2020 was 142 tonnes, lower than in the high-use European countries Spain and Italy, but relatively close to the United Kingdom’s estimated use of 193 tonnes in 2022.
AMR is a problem of our own making; as a direct consequence of the inappropriate use of antibiotics in a drive to produce cheap meat, fish, eggs and dairy foods, on an industrial scale. The most effective way to tackle AMR and achieve optimal health for people, animals and the planet, is to change the way we live and eat; reducing antibiotic use in humans and animals. The widespread adoption of a vegan diet would remove the factory farms that are currently the breeding grounds for these deadly superbugs.
FAQs
What is antimicrobial resistance (AMR) and why is it a danger?
Antimicrobial resistance (AMR) refers to the ability of microorganisms to withstand antimicrobial treatments – antibiotics. It occurs when an antibiotic can no longer stop bacterial growth leaving resistant ‘superbugs’ able to live and multiply unaffected. This is happening because antibiotics have been overused in people and farmed animals. It’s a danger to all because antibiotic-resistant bacteria can spread between people. This can result in new infectious diseases that are more difficult (potentially impossible) to treat.
Is it too late to stop this apocalyptic scenario?
Not quite, but it could soon be. Global livestock antibiotic use is forecast to increase by eight per cent by 2030 and nearly double in Brazil, Russia, India, China and South Africa. Dr David Brown, director at Antibiotic Research UK, told the Guardian newspaper: “I think we have got a 50-50 chance of salvaging the most important antibiotics, but we need to stop agriculture* from ruining it again.”*Dr Brown is referring to the overuse of antibiotics in farmed animals ruining the chance of antibiotics working effectively.
How are bacteria becoming antibiotic resistant?
Antibiotic resistance occurs when naturally occurring random DNA mutations in bacteria help them to withstand antimicrobial treatment. If a mutation enables a single bacterium to survive, while all others die, it will go on to reproduce, spreading and taking its new resistance gene with it like an accessory, enabling it to survive the hostile environment – the genetic equivalent of a stab-vest! In addition, resistance genes may be transferred from one bug to another in a transferable package called a plasmid.
Every time an antibiotic is used, it offers bugs the opportunity to find ways to resist it. Exposure to antibiotics, therefore, provides selective pressure, which makes any surviving bacteria likely to be resistant.In summary, the more antibiotics are used in people and farmed animals, the more likely it is that some will become resistant so that they are no longer killed by the drug. Worse still, bacteria can pass on their resistance to other species of bacteria.
Is antibiotic resistance in farmed animals, causing resistance in human infections?
While some resistant infections in people are probably caused by the misuse of antibiotics in humans, others are due to their misuse in farmed animals. Scientists say, for example, that farm antibiotic use is the principal cause of resistance in human Campylobacter and Salmonella infections and has contributed to resistance in E. coli, enterococcal and other infections. Furthermore, resistance to some critically important antibiotics has been driven by their inappropriate use in both humans and animals. Resistant livestock-associated strains of MRSA infecting humans is also a developing problem.
Farm use of antibiotics is driving up levels of resistance, leading to new superbugs. Most public health experts agree that resistant bacteria are created in farmed animals by antibiotic use and that some of these are being transmitted to people. Find out more here.
How do antibiotic-resistant bacteria in farmed animals spread to people?
Antibiotic-resistant bacteria in farmed animals can pass to people on foods such as meat, fish, eggs and dairy, but also by direct contact or environmental contamination. For example, animal manure is used to fertilise crop fields, which means that bacteria are literally spread on the soil used to grow food!
For Campylobacter, contaminated chicken is the main source and for Salmonella, the most common sources are contaminated chicken, eggs, pork and beef.
Most E. coli strains are harmless and live in the gut of humans and other animals without causing problems. However, verotoxigenic E. coli produces a toxin that can cause serious illness. Cattle are a major source of verotoxigenic E. coli and resistant strains may spread to people via contaminated beef. Infection may cause diarrhoeal disease in humans ranging from mild gastroenteritis to severe bloody diarrhoea and in some, can develop into a serious, potentially fatal illness.
Livestock-associated methicillin-resistant Staphylococcus aureus (LA-MRSA) is widespread in European pig production but has also been detected in milk from Europe, Israel, China and Brazil. People who have prolonged, repeated contact with affected livestock are at a higher risk of becoming infected (or colonised) with LA-MRSA but in the United Kingdom, for example, LA-MRSA has been found in retail beef, pig and poultry meat.Raw meat, poultry and fish have been identified as a major source of exposure of humans to AMR bacteria, with resistance to drugs categorised by the WHO as critically important antimicrobials. The WHO recommends an overall reduction in the use of all classes of medically important antimicrobials in farmed animals and complete restriction (ie a total ban) on using medically important antimicrobials in farmed animals for growth promotion or disease prevention.
What is MRSA?
Methicillin-resistant Staphylococcus aureus (MRSA) is a group of Gram-positive bacteria resistant to numerous beta-lactam antibiotics (a broad class of antibiotics) including methicillin, amoxicillin, penicillin and oxacillin, making infection with MRSA a challenge to treat.
S. aureus is commonly found in the nose and skin of humans. Both S. aureus and MRSA can live harmlessly on the skin (usually in the nose, armpits, groin or buttocks). Healthy people are usually unaware that they are carriers but may suffer from minor skin infections such as boils, pimples, impetigo, abscesses or wound infections.
However, S. aureus is an opportunist pathogen and if it gets further into your body, it can cause more serious infections leading to septicaemia (blood poisoning), pneumonia (lung infection), osteomyelitis (bone infection), endocarditis (heart valve infection), urinary tract infection (eg bladder infection) or septic bursitis (small fluid-filled sacs under the skin).
Information showing how common MRSA is in most African countries is scarce. In a few surveys, the prevalence of MRSA in Uganda has been found to range from as low as two per cent to as high as 41 per cent. Previous studies at Mulago National Hospital showed that 28.7 per cent of surgical site infections were due to S. aureus and of these 31.5 per cent were due to MRSA.
MRSA is a problem in hospitals because there is an increased risk that it will get into a wound and the blood will become infected. In hospitals, for example, there may be more chance the bacteria can spread from person to person via towels, sheets, razors, door handles, sinks, floors and skin-to-skin – but, of course, it also has more chance to enter the body and invade the bloodstream through broken or damaged skin or during medical procedures, causing infections and resulting in conditions that range from mild to life-threatening.
MRSA is mainly spread between people by direct skin-to-skin contact, although it can also be spread through dust and contaminated equipment and surroundings. However, strains of MRSA are emerging from farm animals – and frighteningly quickly. The bacterium that can cause staph skin infections can divide every half-hour in optimum conditions. Theoretically, a single cell can form a colony of more than a million cells in 10 hours. Although largely played down by the meat industry, antibiotic-resistant bacteria from livestock pose a deadly risk to people.
Are the last antibiotics starting to fail?
A number of different strains of MRSA have emerged in farmed animals in recent years, which can colonise and multiply on most species, including humans. The most common of these is livestock-associated methicillin-resistant Staphylococcus aureus sequence type 398 (LA-MRSA ST398), responsible for the massive colonisation of livestock and food products as well as infections in humans worldwide.
The spread of LA-MRSA ST398 throughout Europe’s pig population in particular (it is also present in poultry and cattle), has led to a growing number of infections in humans. Although workers in direct contact with livestock are most at risk, MRSA ST398 can also pass from person to person. There is a real danger that it will spread widely in livestock unless changes in farm antibiotic use are introduced urgently.The pig industry continues to downplay the risk to human health but if MRSA infection levels continue to rise in pigs, it follows that infections in humans will rise too.
How is pig farming linked to MRSA?
A number of different strains of MRSA have emerged in farmed animals in recent years, which can colonise and multiply on most species, including humans. The most common of these is livestock-associated methicillin-resistant Staphylococcus aureus sequence type 398 (LA-MRSA ST398), responsible for the massive colonisation of livestock and food products as well as infections in humans worldwide.
The spread of LA-MRSA ST398 throughout Europe’s pig population in particular (it is also present in poultry and cattle), has led to a growing number of infections in humans. Although workers in direct contact with livestock are most at risk, MRSA ST398 can also pass from person to person. There is a real danger that it will spread widely in livestock unless changes in farm antibiotic use are introduced urgently.The pig industry continues to downplay the risk to human health but if MRSA infection levels continue to rise in pigs, it follows that infections in humans will rise too.
Are the last antibiotics starting to fail?
A last-line antibiotic called colistin is used when all else has failed. It’s an old drug, introduced in 1959, and has been used sparingly in people because it can be toxic to the kidneys and nervous system. Because it hasn’t been used much, bacteria had not developed resistance to it – until recently due to its prolific overuse in farmed animals. Viva! filmed evidence of colistin use in a UK pig farm in 2016.
In 2015, colistin-resistant E. coli were discovered in a pig in China. Scientists then tested samples from other animals as they were slaughtered, retail meat from supermarkets and street markets and samples previously collected between 2011 and 2014 from patients in two hospitals. The gene they discovered, called mcr-1, which causes resistance to colistin, was present in 15 per cent of pork and chicken meat tested, 21 per cent pigs in slaughterhouses and in one per cent of samples from hospital patients.
Worryingly, the mcr-1 gene was found on a plasmid, these are small pieces of DNA that are not part of a bacteria’s chromosome and are capable of carrying so-called ‘accessory genes’. Plasmids move freely around the bacterial world, hopping from one bacterium to another. This so-called ‘horizontal gene transfer’ rang alarm bells across the scientific community everywhere as it not only heralded the breach of the last group of antibiotics available to humans but opened up the possibility of AMR spreading even faster. Bacteria that carry these mobilised colistin-resistance genes have more recently been referred to as ‘jumping superbugs’!
The mcr-1 gene spread fast and has been found in more than 70 countries across five continents, in numerous species across the world and has been reported among human samples from 29 countries. In 2016, a second gene for colistin-resistance, mcr-2, was found in E. coli taken from pigs and cows in Belgium, then in 2017, mcr-3 was identified in E. coli from pigs in China. Many more mcr gene variants have been identified, some retrospectively. In 2020, mrc-10, was found in animals, humans and the environment – scientists said it may have been spreading for some time globally undetected. These mcr genes are now found worldwide, threatening the therapeutic effectiveness of colistin against multidrug-resistant bacteria that are untreatable with standard antibiotics.Resistance to colistin has happened because of its gross overuse in thousands of millions of animals. It’s cheap and has been used to promote growth and combat disease in filthy, overcrowded factory farms. Although now banned as a growth promoter in some countries, others continue to use it to treat infection. Scientists are unsure if this late action can curb the spread of resistance genes – it could simply be closing the barn door after the horse has bolted! Many scientists would like to see a complete ban on the use of this last-line antibiotic in farmed animals.
Why are farmed animals given antibiotics?
Antibiotics are given to both treat existing disease and to prevent it. Like us, animals are more likely to become ill if they are stressed, overworked or kept in filthy, overcrowded conditions. It’s difficult to think of a place that fits those criteria more than a factory farm. Viva! has filmed at dozens of pig and chicken farms over the past decades and found suffering, filth and degradation at them all. It is little wonder that these animals become ill.
However, antibiotic use is increasing in farmed animals. It’s not being reduced or prohibited because factory farming would collapse without it. Due to the increasing global demand for meat, it’s predicted that between 2020 and 2030, antibiotic use in cattle, sheep, chicken and pigs worldwide will increase by eight per cent, when it should be falling.
A report from the World Organisation for Animal Health (OIE) in 2019 found that 45 countries out of the 155 that provided data are still giving antibiotics to animals as a way of fattening them up, a practice that is banned in many parts of the world. Key antimicrobials, classified by the WHO as ‘highest priority critically important antimicrobials’, including colistin, continue to be used routinely in several regions for this purpose.Perhaps the ultimate irony is the fact that without antibiotics factory farms could not exist, yet once antibiotic resistance is complete the animals on those farms will also not respond to drugs. It will mean the end of factory farming, but by then it would also herald the post-antibiotic age for the human race.
How many antibiotics are given to farmed animals globally and in Uganda?
Three-quarters of all antibiotics sold globally are used in animals raised for food. The US and China are the largest users of antibiotics for food production. The estimated annual consumption of antimicrobials in Uganda in 2020 was 142 tonnes, lower than in the high-use European countries Spain and Italy, but relatively close to the United Kingdom’s estimated use of 193 tonnes in 2022.
Are antibiotics still used as growth promoters in pigs?
Antibiotics are used in farmed animals for three reasons to promote growth, to treat disease (therapeutic use) and to prevent disease (prophylactic use).
In some countries, pigs are fed antibiotics to make them grow faster. Administering low doses improves growth rate, reduces mortality and morbidity and improves reproductive performance. This type of antibiotic use is referred to as sub-therapeutic use and the widespread practice of using antibiotics to promote growth in livestock for many years has contributed to the emergence of antibiotic-resistant superbugs.
A European Union-wide ban on the use of antibiotics as growth promoters in animal feed came into effect in 2006, many other countries have also banned their use as growth promoters but in least 41 countries, antibiotics are still being used in farmed animals as a way of fattening them up, according to the World Organisation of Animal Health.
Intensive farms make ideal breeding grounds for bugs – the high stocking density, stress and the low level of genetic diversity all increase the potential for the spread of diseases among animals. To stop this, factory farms often use high levels of antibiotics as a preventative measure rather than a cure. So, many factory-farmed pigs are routinely fed antibiotics, even when they are healthy. The large amount of antibiotics used in factory farming is a significant cause of the resistance of many common bacteria to the antibiotics relied on to treat infections in humans.
Is antibiotic resistance even worse in poorer nations?
Over the last few decades, a large increase in meat production has occurred in developing countries – especially for poultry and pork. This is largely due to population growth, urbanisation and increasing income levels, mirroring what happened in developed countries over the past decades. Inevitably, this led to factory farming and the overcrowding of animals in turn, led to the increased use of antibiotics. Currently, the global consumption of antimicrobials is predicted to increase by eight per cent by 2030.
In many developing countries, antibiotics are not only used to treat disease in farmed animals but to prevent it and also for growth promotion. Additionally, water is frequently contaminated with resistant bacteria – both by faecal contamination from people (poor sanitation) and animal manure. This contaminated water then recirculates to people and farmed animals given antibiotics, which then allows even more resistance to develop and spread. Consequently, most gastrointestinal diseases such as gastroenteritis, salmonellosis, shigellosis, cholera, listeriosis, campylobacteriosis and yersiniosis are caused via water or food contaminated with faeces of animals or people. The large volumes of antibiotics used in livestock in developing countries are contributing to the problem of AMR. Unfortunately, AMR does not recognise geographic borders – we all share one planet. The most effective way to tackle AMR and achieve optimal health for people, animals and our environment is to change the way we live and eat, reducing antibiotic use in humans and animals.
Why aren’t drug companies working on new antibiotics?
Some drug companies are attempting to develop new antibiotics, but progress is very slow. The development of new antibiotics is inadequate to address the mounting threat of antibiotic resistance, according to the WHO.
The problem is new products require a lengthy pathway to approval, incur high costs and have low success rates. It currently takes around 10 to 15 years to progress an antibiotic candidate from the preclinical to the clinical stages. For antibiotics in existing classes, only one out of every 15 drugs in development will reach patients and for new classes of antibiotics, only one in 30 will reach patients.
This means many pharmaceutical companies would rather focus on developing other treatments that have better profit margins as they only recoup the money used to develop new drugs when they sell those drugs. While this works well for medicines used to treat cancer, diabetes, chronic pain and asthma, it’s not so effective when it comes to antibiotics. So, there is less incentive to stimulate new investment in antibiotic research and development.“Time is running out to get ahead of antimicrobial resistance, the pace and success of innovation is far below what we need to secure the gains of modern medicine against age-old but devastating conditions like neonatal sepsis,” said Dr Haileyesus Getahun, WHO Director of AMR Global Coordination.
Why aren’t the drug companies limiting antibiotics for farmed animals?
Money. Any reduction in antibiotic usage will also reduce profits accordingly. In fact, the industry actively campaigns to keep antibiotics being used in the farming industry – and promote even more being produced and distributed.
A joint investigation by the Guardian and the Bureau of Investigative Journalism found that Elanco (who account for 13 per cent of the veterinary pharmaceuticals and operates in more than 70 countries) is using slick advertising campaigns on social media to downplay consumer concerns over giving antibiotics to animals.
All too often, the livestock industry dismisses the claim that the overuse of antibiotics in intensive farming adds to the serious public health threat from antibiotic resistance describing it as a ‘myth’, despite the wealth of evidence to the contrary.Despite accepting that improving the conditions in which animals are farmed can result in significant improvements in antibiotic use, official bodies largely continue to support the status quo.
Why aren’t vets prescribing fewer antibiotics?
Like doctors being encouraged to prescribe fewer antibiotics to people vets have also been encouraged to prescribe fewer antibiotics to farmed animals. Some surely are. However, those working within farmed animal practices rely on the custom of farmers and if they refuse to give out antibiotics those farmers could go elsewhere. Vets are aware that factory farming practices drive illness and disease and so increase antibiotic usage yet continue to prescribe drugs to treat avoidable diseases and illnesses. It is also unclear how many vets have ties to pharmaceutical companies.
How about just eating organic meat?
Free range, organic or higher-welfare indoor farming, may use lower levels of antibiotics but it’s a myth that organic farming is antibiotic-free. Antibiotics will be given to animals in organic farming on the advice of vets. Meat from organic animals cannot be sold if the animal is receiving antibiotics or for a period afterward, but organic farming still plays its part in driving antibiotic resistance.Whilst welfare on less intensive systems can be better (although not always) there are other issues to consider. Extensive farming takes up a lot more room and there simply isn’t enough space in the world to farm all the animals we currently do in less intensive systems. Organic animals tend to be slaughtered at a later age than intensively farmed ones, so often more feed will need to be produced for organic herds. And, of course, all animals – whether organic or factory-farmed – end up at the abattoir for something that we don’t even need and that harms our health.
Will being vegan protect me against antibiotic resistance?
Unfortunately, being vegan will not stop you falling victim to an untreatable infection if antibiotics stop working. However, going and being vegan means that you are healthier and less likely to get ill. For example, 95 per cent of food poisoning cases are caused by consuming animal products. Also, as the risk of antibiotic resistance increases each time an antibiotic is used, as a vegan, it means that no animals will be raised for meat, fish, dairy or eggs in your name and so fewer antibiotics will be used. The more of us who reject factory farming and choose a kinder future will help protect us all. Being vegan is the best chance we have to collectively prevent reaching the point of no return. In fact, it may be our only chance.

